Chronic Myelomonocytic Leukemia (CMML) and Myeloproliferative Neoplasms (MPNs) are disorders affecting the blood and bone marrow, but they have distinct characteristics and treatment approaches. Differentiating between them is important for accurate diagnosis and appropriate management. Let’s understand the comprehensive distinctions between both disorders:
Disease Overview:
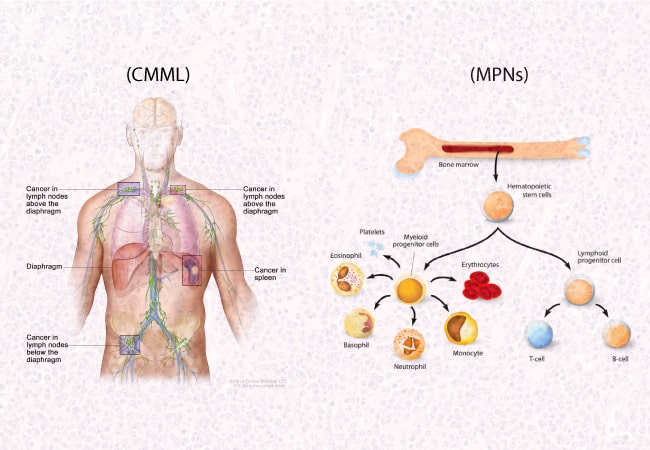
CMML: CMML is a type of leukemia characterized by the abnormal growth of blood cells, particularly myelomonocytes, in the bone marrow and blood. It has features of both myelodysplastic syndromes (MDS) and myeloproliferative neoplasms (MPNs).
MPNs: MPNs are a group of blood disorders where the bone marrow produces too many blood cells. The main types include polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF).
Cell Lineage Involvement:
CMML: CMML primarily affects myeloid cells, specifically myelomonocytes, which are a type of white blood cell (WBC).
MPNs: MPNs involve abnormal proliferation of various types of blood cells, such as red blood cells (in PV), platelets (in ET), or megakaryocytes (in PMF).
Genetic Mutations:
CMML: Common mutations associated with CMML include mutations in genes like TET2, ASXL1, SRSF2, and RUNX1, among others.
MPNs: Different MPNs have distinct genetic mutations. For instance, PV is commonly associated with the JAK2V617F mutation, while ET and PMF may have mutations in JAK2, CALR, or MPL genes.
Symptoms and Complications:
CMML: Symptoms of CMML may include frequent infections, fatigue, easy bruising or bleeding, anemia, and enlarged spleen. It can progress to acute myeloid leukemia (AML).
MPNs: Symptoms vary depending on the specific MPN but may include dizziness, headache, itching (especially after a hot shower in PV), and abdominal discomfort due to an enlarged spleen.
Diagnosis and Prognosis:
CMML: Diagnosis of CMML involves a combination of bone marrow biopsy, blood tests, and genetic analysis to confirm the existence of abnormal myelomonocytes and genetic mutations.
MPNs: Diagnosis of MPNs typically involves blood tests, bone marrow biopsy, and genetic testing to identify specific mutations associated with each subtype.
Treatment Approaches:
CMML: Treatment options for CMML include Inqovi, supportive care, such as blood transfusions and growth factors, as well as chemotherapy, hypomethylating agents, and stem cell transplantation for eligible patients.
MPNs: Treatment for MPNs aims to manage symptoms and reduce the risk of complications. This may include medications to control blood cell counts (e.g., hydroxyurea), blood thinners, and occasionally, stem cell transplantation for high-risk cases.
In conclusion, while both CMML and MPNs involve abnormalities in blood cell production, they differ in their cell lineage involvement, genetic mutations, symptoms, and treatment approaches. Accurate diagnosis by a hematologist/oncologist is essential for determining the appropriate management plan tailored to each patient’s condition.
References:
https://www.lls.org/myeloproliferative-neoplasms
https://bloodcancer.org.uk/understanding-blood-cancer/blood-cancer-types/
https://www.uptodate.com/contents/chronic-myelomonocytic-leukemia-clinical-features-evaluation-and-diagnosis